Total shoulder replacement is a beneficial procedure for treatment of severe stiffness, pain, and immobility that occurs as a result of end-stage degenerative shoulder joint arthritis. The goals of this surgery are to give the patient relief from pain, restore motion, function, and strength of the joint, and to aid in the return to normal activities. Following a total shoulder replacement procedure, most people return to sports they enjoy, such as golf, tennis, swimming, and racke t ball.
t ball.
When shoulder arthritis occurs, the normally smooth cartilage surfaces of the shoulder joint erode away, denying the ball and socket smooth gliding against one another. When cartilage disappears, the result is a “bone on bone” joint, which leads to debilitating pain and loss of mobility.
Types of Shoulder Replacement
- Open surgery: The total shoulder replacement open surgery involves removal of the damaged humeral head, called the joint ball, and replacement of that with a metal ball. Incisions are made at the upper arm and the front of the shoulder. Also, a new smooth plastic surface is placed on the upper arm bone, which is referred to as the socket. The metal-on-plastic allows for a full functioning joint.
- Hemi-replacement: With a partial shoulder replacement (called a hemi-replacement), the ball is the only component replaced.
- Minimally invasive arthroplasty: For patients who have shoulder conditions with diseased ligaments, tendons, and/or muscles, a minimally invasive shoulder arthroplasty is done. This works well when the patient has a torn rotator cuff or labral tear.
- Reverse shoulder replacement: A new type of surgery to replace the shoulder joint is the reverse shoulder replacement. This surgery allows the ball of the joint to be positioned on the patient’s own socket, and the plastic socket is placed on the humerus bone. This reverse design allows the ball to rest against the socket rather than be positioned deep into the socket. The surrounding tendons hold the ball in place and allow for movement. The reverse shoulder replacement gives the shoulder more stability, allowing the shoulder to be moved by the deltoid muscle rather than the rotator cuff, which is perfect for patients who have damage to this structure.
The Open Procedure
During the open procedure, the orthopedic surgeon separates the deltoid and pectoral muscles to visualize the sur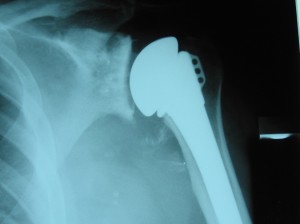 gical area. Also, the rotator cuff is opened by cutting the front muscles so the surgeon can see to manipulate the ball and socket of the shoulder joint. Once the arthritic regions are removed, the surgeon then inserts the implant ball, socket, and stem components. Once positioned, the area is closed by suturing up the rotator cuff muscle. A bandage is applied over the surgical incisions, and it must be kept clean and dry.
gical area. Also, the rotator cuff is opened by cutting the front muscles so the surgeon can see to manipulate the ball and socket of the shoulder joint. Once the arthritic regions are removed, the surgeon then inserts the implant ball, socket, and stem components. Once positioned, the area is closed by suturing up the rotator cuff muscle. A bandage is applied over the surgical incisions, and it must be kept clean and dry.
Either regional or general anesthesia (or both) is used for the total shoulder replacement procedure. Most patients are operated on in the beach-chair position. The implant materials are a metal ball and a plastic polyethylene socket.
Candidates for Shoulder Replacement Surgery
A shoulder replacement procedure is indicated for patients who have severe shoulder pain due to arthritis that is not controlled with conservative measures, such as injections and medications. Also, loss of range of motion and stiffness are reasons for shoulder surgery. These problems occur when the ball and socket rub against each other when there is not enough cartilage for smooth gliding.
To determine if the patient is a candidate for shoulder joint replacement, the doctor will order a magnetic resonance imaging (MRI) scan, x-rays, and possibly, a computed tomography (CT) scan. If nerve damage is suspected, a nerve conduction test (EMG) is done. For patients with ankylosing spondylitis of the shoulder, replacement alleviates the stiffness and improves overall joint function and mobility.
Patients who are not good candidates for a shoulder replacement procedure include those with:
- Symptoms that are not severe.
- Loss or paralysis of the deltoid muscles and rotator cuff.
- Active infection.
- Progressive nervous system disease.
Recovery/Rehabilitation
Once the patient leaves the operating room, he or she is transferred to the recovery room, and the surgical arm is immobilized in a removal canvas sling. Usually, the patient wakes up from surgery in the recovery room, but pain will be minimal. Once stabilized, the patient is transferred to a hospital room. Based on stability of the implant and shoulder range of motion, physical therapy begins the following day (the first postoperative day).
During the early rehabilitation phase, the patient uses the sling to allow the tendons to heal without injury. The sling is only removed for showering and for therapeutic exercises. The physical therapist has the patient use the wrist and hand immediately following surgery, but use of the whole arm and shoulder doesn’t begin until approximately six to eight weeks following the procedure. Recovery landmarks include:
- Three months post-surgery – Most people have around 50 percent of mobility but notice slight weakness of the shoulder.
- Six months post-surgery – Most patients do not have pain. Strength and motion is about 66 percent of normal ability.
- Twelve months post-surgery – Around 95 percent of patients are pain-free, and it is rate for someone to have significant strength or mobility issues.
Possible Complications
As with any surgery, a total shoulder replacement does have a few complications. These include:





